Understanding Transfusion Medicine
Transfusion medicine is a vital branch of healthcare focusing on the process of transferring blood and its components to patients in need. This medical specialty plays a crucial role in saving lives and enhancing patient outcomes across various clinical scenarios. Blood transfusions are primarily employed in cases of severe blood loss due to trauma, surgery, or medical conditions such as anemia and clotting disorders. The timely administration of blood can significantly improve the prognosis for patients experiencing significant hemorrhage or undergoing invasive procedures.
In transfusion medicine, various blood components can be transfused, including red blood cells, platelets, plasma, and clotting factors. Each of these components serves specific therapeutic purposes and can be used independently or in combination based on the patient’s individual clinical needs. For instance, red blood cell transfusions are predominantly administered to correct anemia and restore adequate oxygen delivery to tissues, while platelets are vital in treating bleeding disorders or conditions that compromise normal platelet function. Plasma transfusion helps in the management of patients with clotting deficiencies, ensuring proper hemostatic function.
As the field of transfusion medicine continues to evolve, ongoing education and professional development are essential for healthcare professionals involved in this critical area of patient care. MedSkillHub offers a continuous professional development (CPD) series that focuses on enhancing the knowledge and skills of medical practitioners in the blood transfusion process. This series covers the latest advancements, best practices, and safety measures in transfusion medicine, ensuring that healthcare providers remain proficient in delivering optimal care to patients needing blood products.
The Blood Donor Process
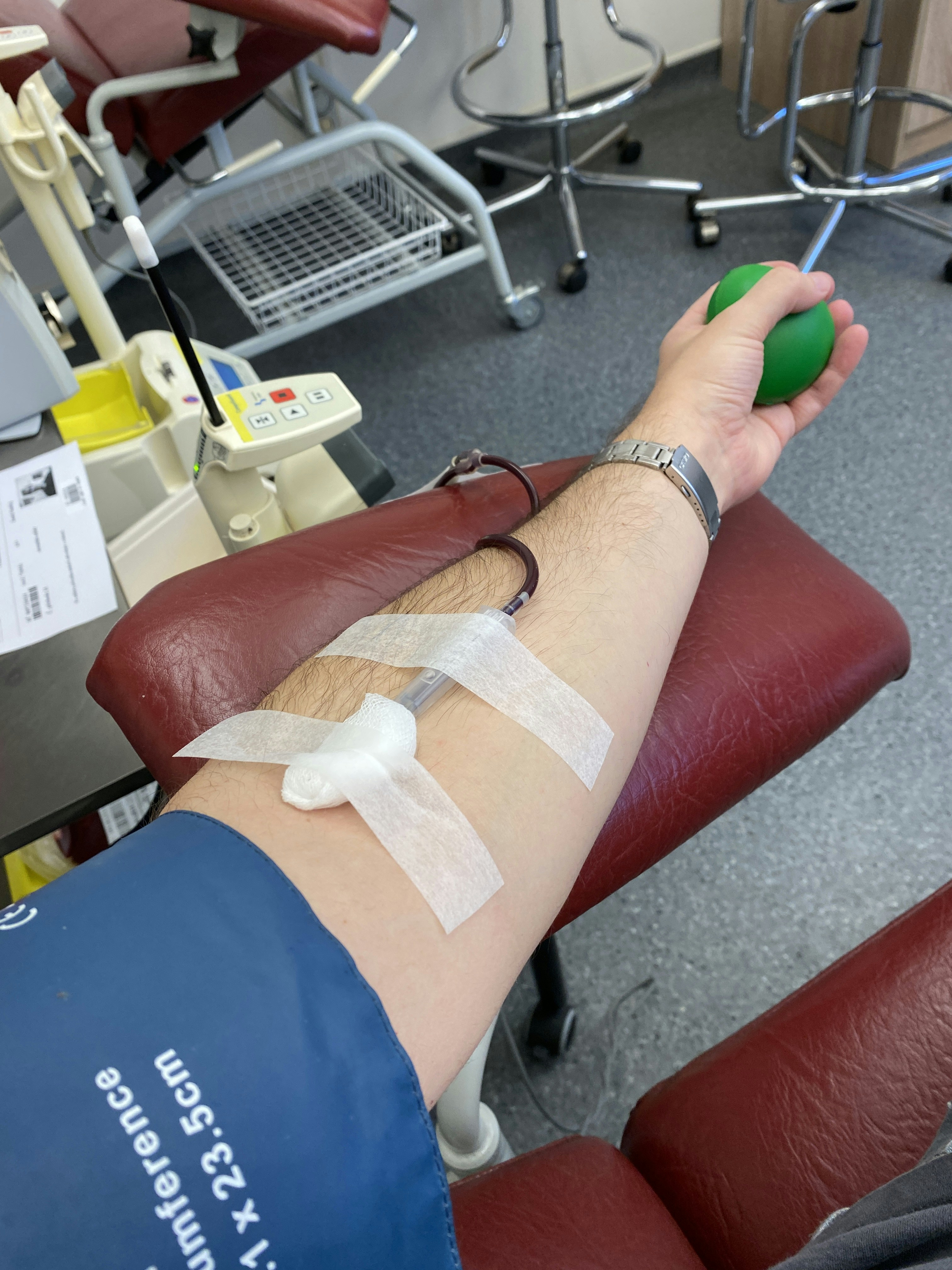
The blood donor process is a pivotal aspect of transfusion medicine, as it represents the very first step in ensuring a stable and diverse supply of blood products for those in need. To become a blood donor, individuals must meet specific qualifications that typically include being at least 17 years old, weighing a minimum of 110 pounds, and being in good general health. Additionally, potential donors are screened for certain risk factors and medical conditions that might disqualify them from donating blood, thereby emphasizing the importance of health and safety in the process.
The collection of blood itself is a straightforward procedure, often taking less than an hour. After registration and screening, donors will provide a small blood sample to check their hemoglobin levels. Once approved, a trained phlebotomist will carefully insert a sterile needle into the donor’s arm to collect approximately one unit of blood, which typically amounts to about 500 milliliters. Throughout the process, donors are encouraged to relax and engage in conversation, which aids in creating a comfortable environment and minimizes anxiety.
Equally important as the procedural aspects of blood donation are donor consent and education. It is crucial that individuals understand the impact of their donation and provide informed consent. Educational materials are often distributed to raise awareness about the need for blood donations, as well as the implications of various blood types. A diverse blood donor pool is essential, as it helps meet the needs of a wide range of patients with different blood type requirements. Blood donation campaigns play a significant role in recruiting donors and informing the public about the necessity of regular donations, thereby reinforcing the idea that every donation can save a life.
Testing and Processing of Donated Blood
Before donated blood can be used for transfusions, it undergoes a series of rigorous tests and processing procedures to ensure its safety and effectiveness for recipients. Screening for infectious diseases is one of the most critical steps in this process. Potentially harmful pathogens such as HIV, Hepatitis B and C, and syphilis must be detected and evaluated. Advanced assays are utilized to confirm the absence of these infectious agents, allowing medical professionals to guarantee the safety of blood transfusions.
In addition to screening for infections, blood type testing is conducted to identify the ABO and Rh(D) blood groups of the donors. This information is vital as incompatible blood transfusions can lead to severe reactions in the recipient. Accurate blood typing ensures that patients receive the correct blood type, thereby minimizing the risk of transfusion complications.
Following these essential tests, the donated blood is processed into its components, which include red blood cells, platelets, and plasma. This separation is achieved through centrifugation, where blood is spun at high speeds to separate the different elements based on their density. Each component has specific applications; for instance, red blood cells are crucial for patients experiencing anemia, while platelets are vital for those undergoing treatments for conditions such as leukemia.
The meticulous testing and processing of blood not only enhance patient safety but also ensure the efficacy of the transfused blood product. Hospitals and blood banks adhere to strict regulatory guidelines and protocols to create a reliable supply of safe blood. This careful approach, backed by scientific testing and processing, underscores the paramount importance of quality control in transfusion medicine.
Transfusion Administration and Monitoring
The administration of blood transfusions is a critical aspect of transfusion medicine, demanding precision and adherence to established protocols. Healthcare professionals are required to follow a series of stringent pre-transfusion checks aimed at ensuring patient safety and the efficacy of the procedure. These checks include confirming the patient’s identity, blood type compatibility, and verifying the blood product’s labeling. It is essential for each member of the healthcare team to meticulously review these elements to minimize the risk of transfusion-related complications.
During the transfusion, continuous monitoring of the patient is imperative. Vital signs are regularly assessed to identify any immediate adverse reactions, which may include fever, chills, or any signs of hemolytic reactions. Such monitoring is not merely a regulatory requirement but a critical element that can facilitate immediate intervention, should complications arise. The recommended protocol typically involves taking baseline vital signs prior to starting the transfusion, followed by periodic checks at specific intervals during and after the procedure.
The management of potential transfusion reactions is another vital component of the transfusion process. Healthcare professionals must be trained to rapidly identify and address these reactions, which can vary from mild to severe. In cases of adverse reactions, established guidelines dictate the immediate response steps, including stopping the transfusion, maintaining venous access, and providing symptomatic treatment as needed. This preparedness is essential for safeguarding patient outcomes and underscores the importance of ongoing education and training in transfusion practices.
Post-transfusion monitoring is equally important, as it allows healthcare providers to observe the patient for delayed reactions that may occur hours or even days after the transfusion. Proper documentation and communication within the healthcare team further enhance the safety and efficacy of transfusion practices, ensuring that every transfusion is administered with the utmost care, thereby reinforcing the commitment to patient safety and high-quality care in transfusion medicine.
